Kudos to everyone in Newport who
turned out at the city council meeting Tuesday
night, and to the city council for passing a resolution asking Brown Health to keep the maternity unit at Newport Hospital open.
It’s crazy we are at this point in the US, where we have to worry about providing something as essential as maternity care to young families. But Newport is not alone. Over two million women of childbearing age in the US live in ‘maternity deserts’ – counties where access to maternity care services is limited or absent. Too many women have to drive fifty or even a hundred miles for maternity care, which is crazy, because everything about labor – the timing, the duration, and the safety or lack thereof – is unpredictable. We are pretty good at identifying pregnancies at high risk, but even low-risk pregnancies can get into life-or-death trouble in an instant, with heartbreak resulting if there isn’t highly sophisticated help right there. Yes, women have been delivering babies without doctors and nurses for millions of years – but before all our fancy technology, we lost up to fifty percent of babies, and twenty percent of their mothers, in or as a result of childbirth. To run a safe and effective maternity unit, you need great maternity nurses who can help most moms have a safe and natural birth. But you also need great doctors – family doctors (some of whom are trained to do caesarian sections), obstetricians, pediatricians and anesthesiologists, and you need those services 24 hours a day, seven days a week. Which is both expensive and logistically difficult, particularly for small maternity units. You need to recruit and retain enough good people to staff such a unit, and they need enough volume so their skills stay sharp, but enough rest so they can think clearly and decisively when needed. And be kind and supportive throughout.
That said, our maternity care situation is made more complicated by the chaos we created when we made healthcare a business. Even though 60 to 70 percent of hospital income is supplied by the government in one form or another, our hospital systems operate independently of the government, with their own governing boards whose only responsibility is to keep hospitals solvent. (Medicaid usually pays for maternity care for about half of the pregnant population. The rest is paid for by private insurance, public employee, and veterans’ insurance, and out of pocket by families via copays and deductibles.) Insurance creates all sorts of rules that make the process complicated. Hospitals have to decide whether what insurance pays them makes the “maternity business” profitable, and compete with one another. Because we treat hospital care as a business, we don’t let hospitals grow too big, so that they will compete because we believe competition drives down prices, a notion that works well for TV sets and tomatoes (absent tariffs, of course) but is fundamentally flawed when we talk about health care, because critical mass matters for staffing and expertise. In a population of one million, we might be able to support enough skilled staff to provide maternity care for the entire population, but only if that staff works under a single umbrella and can be moved from place to place to fill in gaps. But when that staff has five different employers and can’t be moved around, when necessary, you get gaps, which is what happens with maternity services. And now the politicians and the lawyers make us balkanize that staff to five different places, having determined that competition is more important than quality maternity care and other medical and health services.
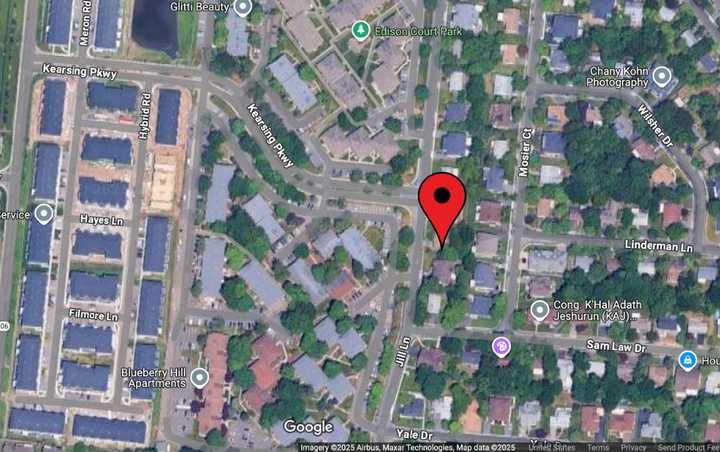
In Newport, that situation is made more difficult by how hospital care is organized. Brown Health aka Lifespan (remember my column about lipstick on a pig, and my worries for the integrity of Newport Hospital when that name change was announced?) has only one maternity unit – Newport. So it doesn’t have any bench at all for maternity care, and its anesthesiologists may not have as much depth of experience in obstetric anesthesiology as those from Women and Infants. Women and Infants has that bench, but they are on the other “team”. One of the best family medicine residency programs in the nation is in Rhode Island, but it’s at Care New England as well, not at Brown Health – though a part of its training is actually run collaboratively between them.
So running a hospital with a maternity unit is likely out of Brown Health/Lifespan’s comfort zone. Everyone awake in health policy knows that the Big Beautiful Bill will cause lots of people with Medicaid to lose insurance, which creates financial risk for Newport’s maternity unit, even though those cuts won’t hit for 18 months and even though pregnant women are still likely to be covered (though perhaps not if they are undocumented) and every uncovered pregnancy represents a big, and sometimes a huge, financial risk for a hospital, which is a big deal, if you are a hospital and your board says your job is to be financially sound ( in addition to caring for your community.) I don’t know where the Brown Health/Lifespan folks live, but if you don’t live in the community you serve, if you didn’t grow up there, the meaning of these decisions is different, regardless of how ethical and well-intentioned you are.
So the challenges are real.
What’s a mother to do? (I’ve waited years to use that line.) The better question is, what’s a community to do?
First, organize and stay organized. I have been at every health policy table in the US that matters, and I can tell you with absolute certainty that the cavalry isn’t coming. The Department of Health, the Attorney General, the Governor and the Congressional Delegation have some and variable leverage, but are not that likely to be able to hold sway over a corporation with a $1.3 billion endowment ( if I am reading their 2022 financial statement correctly, the last one I could find on line) alone, remembering that I was the Director of the Department of Health in 2013 and failed miserably in my attempt to keep the wonderful maternity unit at Westerly Hospital open. (That community was great then, but they weren’t quite organized or powerful enough to help me back down the business guys and the lawyers.) Newport is different. You have the House and Senate Finance Chairs in your state delegation, both wonderful people who can help. But they can’t do this alone either.
Second, explore options. Learn about how other small hospitals keep their maternity units open. Talk to Landmark, which has one of the best small units in the nation, run by an amazing family doctor named Susanna McGee, MD. Talk to Care New England. Talk to South County (which seems to be in a bit of a mess lately) and Kent. Think about starting a family medicine residency at Newport, which would address maternity care and secure the primary care workforce, all at the same time.
Third, follow the money. Is this a Medicaid, Blue Cross, United, Tufts, or NHPRI reimbursement problem – or all of the above? (Remember the bulk of health care financing is via public money, and reimbursement levels can be changed to address real problems by working with the legislature and sometimes, with the Federal delegation.) Think about financing Newport itself could bring to the table, via the tourist industry or other public revenues. I’m betting money alone won’t fix what I’m guessing is a bandwidth problem, but the truth is that there is no mission without a little margin, understanding that the mission/margin is a distinction that is way too often finessed by administrators in the service of their own positions and at the expense of the public’s health.
It’s crazy that Newport has to join so many other places in the US to defend the holy act of women giving birth. But Newport is better equipped to do this than many other places. Margaret Mead reminded us that a small group of thoughtful, committed citizens can change the world. A small group, strong arms, and outstretched hands may be able to save the day here with leadership, community ,and commitment.
Editor’s Note – Dr. Michael Fine is the coeditor of
Maternal Morbidity and Mortality, Clinicians, and Public Health: An
AJPH
Supplement
, which came out in 2024.
Michael Fine, MD, is a writer, community organizer, and family physician. He is the Chief Health Strategist for the City of Central Falls, RI, and a former Director of the Rhode Island Department of Health from 2011 to 2015. He is currently the Board Vice Chair and Co-Founder of the Scituate Health Alliance, and is the recipient of the Barbara Starfield Award, the John Cunningham Award, and the June Rockwell Levy Public Service Award. He is the author of several books, medical, novels and short stories, including On Medicine and Colonialism, Rhode Island Stories, and The Bull and Other Stories, You can learn more about Michael at
www.michaelfinemd.com
.
More from What’sUpNewp
Join 300+ Newport County neighbors supporting local journalism through the What’sUpNewp Press Club
Morning Notes: Kenny Loggins to appear at newportFILM’s ‘Conviction of the Heart’ screening
Sakonnet Vineyard celebrates Little Compton’s 350th Anniversary with Summer Concert Series and Folk Festival
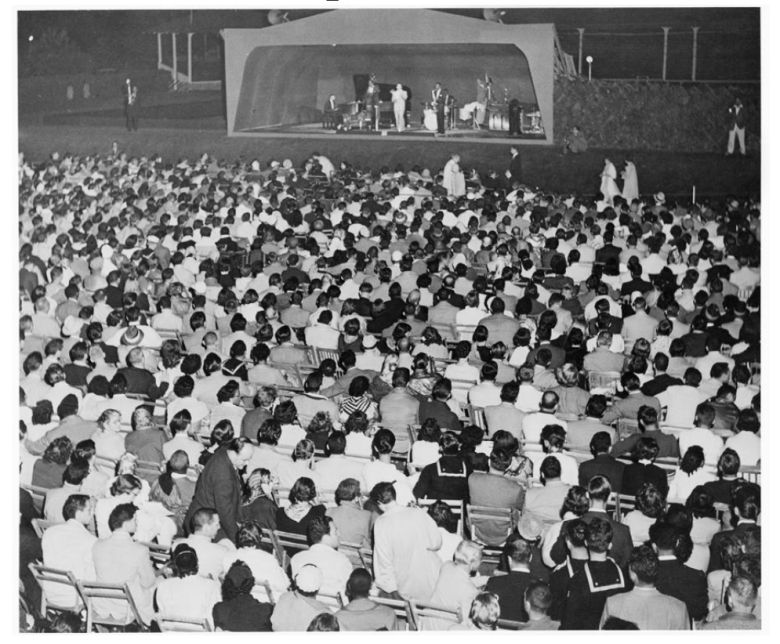
On This Day In Newport History: July 17, 1954 – First Newport Jazz Festival Held
Something went wrong. Please refresh the page and/or try again.